
Translating research into care: Norvell supports veterans with limb loss

For more than two decades, Research Associate Professor Daniel C. Norvell, MPT, PhD, has been helping clinicians and patients make more informed, personalized decisions in the face of lower-limb amputation. A former U.S. Army physical therapist and University of Washington-trained epidemiologist, Dr. Norvell leads the LEADER program—Lower Extremity Amputation Decision Enhancement Research—at the VA Center for Limb Loss and MoBility (CLiMB).

After a VA predoctoral fellowship, Dr. Norvell began collaborating with his mentor and colleague Dr. Joe Czerniecki, now a professor emeritus. They were later joined by key colleagues Drs. Aaron Turner, Rhonda Williams, and Kevin Hakimi. Together, the team developed AMPREDICT, a set of predictive models for mobility, mortality, and reamputation risk following lower extremity amputation at various possible amputation levels. Each amputation level has a tradeoff. Lower amputations may increase the chance that a patient will walk again, however, a low amputation may be harder to heal and require another surgery. The possible outcomes are individual to each patient. That’s why tools such as AMPREDICT are crucial. The decision on how much of a limb to amputate has profound implications for patients’ health, mobility and quality of life after amputation.
AMPREDICT was based on studies conducted between 2005 and 2014. By 2017, physicians around the world began asking the LEADER team if they had a risk calculator to facilitate the clinical application of the models. At this time, Dr. Alison Henderson, a clinical psychologist and implementation scientist joined the team, and helped lead the effort to create the AMPREDICT Decision Support Tool (www.ampdecide.org) to aid providers in choosing the most appropriate amputation level.
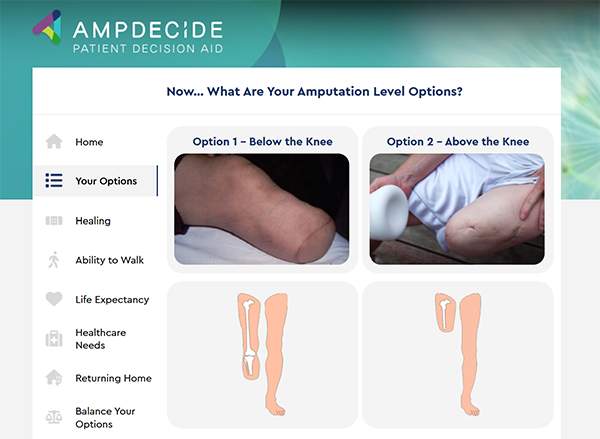
To complement the provider-facing tool, the team developed AMPDECIDE. This tool helps patients and providers make shared decisions by helping Veterans evaluate the risks and benefits of each amputation level based on their personal goals. Today, the AMPREDICT Decision Support Tool and AMPDECIDE Patient Decision Aids are used by more than 6,000 providers in 79 countries. Providers have noted several benefits to using the tools, including enhancing patient/provider shared decision-making, improving patient knowledge and expectations, and facilitating communication among providers.
These tools have been recognized both nationally by the VA and internationally, including a top-read feature in Vascular News. A group of providers in Denmark is currently translating AMPDECIDE for international use.
In a recent voluntary survey of 34 VA providers, nearly 80% reported using the AMPREDICT and AMPDECIDE tools regularly in clinical care. Additionally, 84% said they would recommend the AMPREDICT tool to colleagues, while 74% would recommend AMPDECIDE aids.
In 2018, the Agency for Healthcare Research and Quality (AHRQ) published a major report highlighting the lack of tools for predicting prosthetic outcomes. This prompted the LEADER team to develop the AMPREDICT PROsthetics model, focused on predicting mobility at the time of prosthesis prescription. In 2023, Drs. David Morgenroth and Beth Halsne joined the team to help translate the model into a web-based tool.
The result is PROPREDICT, a tool launched in April 2025 and available at www.prodecide.org. It is already in use by over 400 VA providers. It supports informed planning around prosthesis prescription and planning patient-centered rehabilitation by predicting a patient’s future mobility. The tool was introduced globally at the June 2025 International Society of Prosthetics and Orthotics (ISPO) symposium, where Dr. Norvell presented alongside Drs. Morgenroth and Halsne. It is now being used in 15 countries.
The team is now focused on integrating AMPREDICT and PROPREDICT into the VA’s electronic health record, allowing providers to access them seamlessly at the point of care. For health researchers with little information technology experience, this phase of the project has been challenging, but the team is rapidly growing their skills in this area.
Reflecting on the journey to create these important tools, Dr. Norvell notes that, “the most rewarding aspect of this work has been the team science and collaboration.” These tools are the result of two decades of work with dozens of core collaborators. “Seeing the global impact makes the years of effort truly worth it,” Dr. Norvell continues.
The LEADER team remains committed to advancing precision rehabilitation and patient-centered care for Veterans with limb loss.
