From private practice to academic innovation: Sports & Spine at UW Medicine
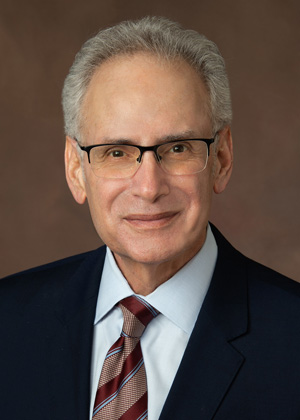
Twenty years ago, leaders at the University of Washington invited Stan Herring, MD, and his talented partners, Stu Weinstein, MD, and Chris Standaert, MD, to bring their private sports medicine experience into an academic setting. Their proposal was simple but ambitious: Could a private practice model thrive within a university and elevate care, training, and research?
The doctors knew that Mark Harrast, MD, a faculty member in the Department of Rehabilitation Medicine, had already established a solid sports medicine foothold at UW Medicine. After thoughtful discussion with many stakeholders, the three doctors gave a definitive “yes” to the idea of coming on board. However, there was one non-negotiable demand: Dr. Herring’s long-time assistant, Sandy Thompson, had to have the opportunity to apply for a position. She did, and they have worked side by side for 38 years.
Today, Dr. Herring is a clinical professor of rehabilitation medicine at the UW Medicine School of Medicine and has led the Department of Rehabilitation Medicine’s Division of Sports & Spine for two decades. In that time, he has received national and international recognition, helped shape youth sports concussion policy, and co-founded The Sports Institute, which works to expand participation and safety in sports. However, Dr. Herring seems more comfortable downplaying his professional accomplishments while emphasizing the contributions that his colleagues and his field have made to sports and spine medicine.
As a physiatrist (also known as a physical medicine and rehabilitation or PM&R doctor), Dr. Herring emphasizes that the division is rooted in the physiatric approach: focusing on function, whole-person care, and interdisciplinary teamwork. The division, which began as a small team, has grown into a thriving group of 19 talented, committed specialists who care for thousands of patients each year.
The division’s mission extends beyond clinical care. Residents in the UW Medicine School of Medicine’s Physical Medicine and Rehabilitation Residency program learn a comprehensive approach to activity-related injuries, including the adjunctive role of procedures such as musculoskeletal ultrasound and spinal injections. The department’s Sports Medicine Fellowship prepares specialists who often remain at UW as faculty or practice at other academic institutions after training. While the division teaches current techniques, Dr. Herring underscores that what makes it distinctive is not interventions alone—it is the philosophy at the heart of the field of PM&R.
The physiatric approach—being part of a team that understands and addresses all components of an injury or illness with a treatment plan focused on restoring function—provides an excellent framework for treating injuries in active people and athletes. “For example,” Dr. Herring said, “when a baseball pitcher has a sore shoulder, many healthcare professionals focus only on that joint, and certainly our physicians thoroughly examine the injured area. However, we also assess other potential contributors to the injury and how they change the biomechanics of throwing, whether it’s an old sprained ankle, torn hamstring, stiff hip, weak core muscles, or an improperly functioning shoulder blade.” In other words, the overworked and painful shoulder is often the victim, while many other structures are the culprits. “Physiatrists don’t just treat an injury—we try to look at all the factors: medical, biomechanical, emotional, and environmental, that made it happen,” Dr. Herring explained. “We think in terms of function, not just symptoms.”
“Patients don’t care how much you know until they know how much you care.”
That broader view, rooted in the biopsychosocial model, considers not only the physical aspects of injury but also the emotional and psychological impacts. As Dr. Herring said, the real issue with many injuries “isn’t just the pain, it’s the suffering.”
Dr. Herring also notes that the doctor-patient relationship is key to helping patients heal. He said, “Patients don’t care how much you know until they know how much you care.”
The division serves a wide range of patients, from children to adults in their 80s and 90s, some of whom still run road races or compete in powerlifting. Others want to continue gardening, walking, or doing chores around the house. The division’s doctors also treat high school, collegiate, Olympic, Paralympic, and professional athletes. No matter what patients may need, UW Medicine sports and spine physiatrists can help assemble a team to get them there. Collaborating closely with specialists including physical therapists, athletic trainers, psychologists, strength and conditioning coaches, and surgical colleagues, physiatrists focus on restoring function and improving quality of life. “There’s no wrong door for us,” Dr. Herring said, referencing sports medicine practices that limit appointments to certain ages or team affiliations. “We try to find the inner athlete in everyone.”
For Dr. Herring, connection is core to care. “I want to know as much as I can about who I am treating. Even the name of their dog,” said Dr. Herring with a grin. Those personal details are not just good customer service. They are essential to a complete medical history. Without asking about a patient’s family, work, sleep, diet, habits, and hobbies, a doctor could miss the key to understanding what a patient’s injury means to them.
Watching patients recover is deeply motivating, he added. Some of his patients are octogenarians who have lost a long-time spouse. For them, a clinic visit can be a bright spot: a reason to dress up, put on their best tie clip or earrings, and connect. “Those moments remind us to slow down and engage for a few minutes more. It reminds us that healing is about people, not just injuries,” Dr. Herring said.
“I treat the Seahawks like I treat you.”
Dr. Herring spent many years as a team physician with the Seattle Seahawks, and patients sometimes ask him to “treat me like a Seahawk.” But these patients have it backwards. Dr. Herring offers the same reply every time: “I treat the Seahawks like I treat you.”
As the division looks toward the future, Dr. Herring recognizes that treating patients one by one isn’t enough. To make a real difference in the nation’s health, the division must embrace its role in public health advocacy and research. Along with sports and recreation-related concussion education, outreach and research, and youth mental health and performance training, Dr. Herring points to efforts led by colleagues in his division such as Clinical Professor Cindy Lin, MD. Her research efforts through The Sports Institute have shown the extraordinary power of prescribing and monitoring exercise in improving the health and welfare of a broad range of individuals while simultaneously driving down healthcare costs. She is currently studying the effects of exercise in conditions ranging from bladder cancer to multiple sclerosis.
“Exercise is a magic potion, yet only about 20 percent of kids and adults get the recommended amount,” Dr. Herring explained. He argues that shaping public policy around topics such as concussion care, youth mental health, and exercise and physical activity is as critical as treating individual patients.
Reflecting on the past 20 years, Dr. Herring sees the principles of the field of physical medicine and rehabilitation as essential to the division’s future. “What makes us unique is the physiatric approach,” he said. “That approach is foundational to how we treat our patients.”
Dr. Herring references the vision statement of the Department of Rehabilitation Medicine, “a world where all people can fully participate and thrive,” and notes, with a smile, that he is all in. And with that, Dr. Herring heads off to his next appointment.